JCROWS.COM
Moxibustion Articles and the ST36 Meridian Point
Leg Three Miles (Stomach 36)
Moxibustion Articles and the ST36 Meridian Point
Leg Three Miles (Stomach 36)
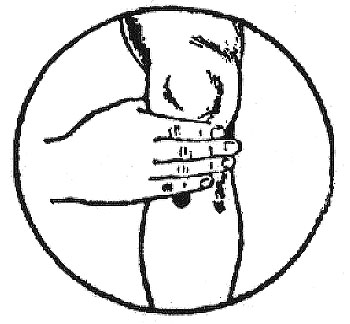
Location: On the front of the leg, one hand width (four fingers) below the kneecap, on the outside, in the depression between the shinbone and the leg muscle. What can go wrong is that you may be locating it somewhat too low on the leg. The point is immediately one hand breadth below the kneecap, so if you'd use something thick, like a finger, you might get half a finger breadth to low. It's at the outside of the bone that's on the front of the lower leg, one finger breadth from the crest of that bone.
Use: Press. A fingernail or thumbnail is particularly suited
for this point, as you will be able to press more closely to the bone and
on a broad range.
Warning: Using this point to go beyond your limits (e.g. overwork)
will damage your health even further.



Maximum Oxygen Uptake AND ST 36
YOSHITO MUKAINO, M.D., SPORTS SCIENCE LABORATORY, FUKUOKA
UNIVERSITY, JAPAN
Translation: Shinjiro Kanazawa, L.Ac., MTOM
Health maintenance, "preventing illness before it shows its symptom" is the core idea in acupuncture and moxibustion theory. Clearly, ancient people had a concept of that stage of illness that comes before illness shows its symptom, and they believed it best to treat illnesses at this stage. This stage is called, in Chinese, "Mi Bing," and in Japanese "Mi Byo," which means "before illness."
"Mi Bing" is closely related to the idea of longevity and moxibustion on the acupuncture point St 36 (stomach 36: Zu San Li in Chinese, Ashi-no-san-ri in Japanese). A Japanese folk tale from the Edo era (1603-1867) about Farmer Manpei tells that when Manpei was asked whether he had any secret to maintaining long life, he answered that he had no secret other than burning moxa on St 36 every day, just as his ancestors had done. It is recorded that Manpei lived 243 years; his wife, Taku, lived 242 and their son, Mankichi, lived 196 years. In recent records, it is well known that Doctor Shimetaro Hara (deceased) used to burn moxa on his St 36 every day and he lived to be over 100 years of age.
A story about St 36 which is very familiar to the Japanese is the first sentence of Haiku Master Basho Matsuo's diary (1689) "Okuno Hosomichi (Narrow Passages In The Back Country)." He writes, "I have sewn a torn part of my undergarments. I have changed the strings of my hat. I have burnt moxa on my St 36. My mind is now totally occupied with the moon over the Matsushima islands..." He was ready for a long walk of 1,500 miles after burning moxa on St 36. This means that our ancestors knew very well that moxibustion on St 36 has the effect of speeding recovery from fatigue.
We studied the effect of stimulation on St 36 in our laboratory by creating a fixed quantity of lower leg fatigue and observing recovery by measuring the successive changes in carbon dioxide partial pressure through the skin. As a result, we found that stimulation on St 36 speeded recovery from fatigue. We presume that the factor of speeding up recovery might be the improvement of the minute circulation of the blood.
Here, I would like to introduce one of my cases that showed an extreme improvement in minute circulation. This was a case of intermittent claudication. The male patient was given an angiogram, which revealed right occluded arteriosclerosis. I could not detect the digital plethysmogram of the right lower leg. The balloon catheter was not attempted to expand his clogged vessel. Prostaglandin and other medications which have strong vasodilation effects were ineffective. In this case, he had intermittent claudication every 50 m (150 ft) when walking. I stimulated his St 36 by injecting physiologic saline subcutaneously every week and he extended his walking distance little by little until finally he could walk without any pain. I did the angiogram again and found the vessel still clogged. This means that even when the large vessel of the lower leg was clogged, needed oxygen for walking was sufficiently supplied. Successive stimulation treatments on St 36 enhanced the development of minute circulation of blood in the lower leg.
Minute circulation of blood is one of the normal factors of Maximum Oxygen Uptake. There is a possibility that stimulating St 36 increases Maximum Oxygen Uptake.It is known that increased Maximum Oxygen Uptake prevents and improves recovery time from diseases caused by lifestyle, such as hypertension and diabetes. Maximumu Oxygen Uptake also decreases the cancer rate. Thus, we could assume that the modern idea of maintaining health by increasing Maximumu Oxygen Uptake is based on the same mechanism as our traditional wisdom for attaining longevity by stimulating St 36.
We could also assume that moxibustion on St 36 has an effect on maintenance and improvement of health in the modern sense, but this has already been proven by the monk Kenko Yoshida, around 1330, who says "If people over 40 years of age do not practice moxibustion on their bodies by burning St 36, they will get flushing (uprising Qi). They should get moxibustion without fail." He pointed out that moxibustion on St 36 is necessary for the maintenance and improvement of health for the person over 40 years of age.
Increasing Maximumu Oxygen Uptake through exercise therapy is a policy of the Japanese government, and it is a modern way of "preventing disease before it shows its symptom." It is essential to remember that the intensity, amount and duration of exercise has to be adequate. In the premodern era, people had to walk, having few or no other means of transportation. In those days life itself provided the amount of exercise that modern exercise therapy suggests people should have. So then, where did our ancestors get the idea that burning moxa on St 36 would "prevent disease before it shows its symptom"?
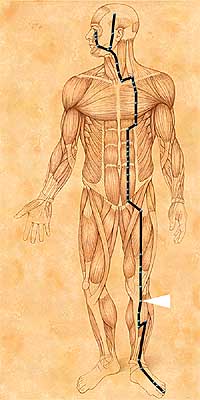
We find the answer in the idea of meridians, which is the basis of the theory of acupuncture and moxibustion. According to this idea, St 36 is located on the network called the Stomach Meridian, and stimulation on St 36 not only stimulates the point but also the entire meridian and stomach organ. According to this classic medical theory, the organ and meridian of the stomach are a part of the foundation of our life energy. Thus, stimulation on St 36 not only affects the leg where St 36 is located, but also affects the health of the whole body.
Moxibustion (Moxa + combustion) is a heat application
treatment on the acupuncture points with the use of a herb called "Moxa".
In moxibustion, usually a grain-size cone of moxa or dry yellow spongy
substance made from a herbal plant "mugwort " is placed on the acupoints
and lit with an incense stick. The burning moxa is then pinched out or
taken away by the therapist before it burns down completely to the skin.
The patient experiences a very comfortable sensation of heat that penetrates
deep into the skin (Direct moxibustion).
Another popular way of using moxa is to burn a moxa cone on the head of
inserted acupuncture needles, or use a cigar-type stick moxa to warm the
acupuncture points at a distance (Indirect moxibustion).
Because of the difference of quality and processing of moxa between Japan
and China, Japanese acupuncturists in general prefer direct moxibustion
while Chinese therapists do indirect moxibustion, especially stick moxa.
It requires a great deal of training for a therapist to master the direct
moxibustion techniques, but it is much more effective than indirect moxibustion.
|
|
 Dr.
Jarvis' Unpublished Notebook Dr.
Jarvis' Unpublished Notebook
-147 hand written pages of advice to correspondents- CD-PDF Format $49.95 ea. Includes Shipping |
| MX101 | Chinese
Traditional Packed Moxa Rolls - used for indirect moxa heat treatment.
Paper covered rolls are approximately 8.3" x 0.75" in diameter.
|
(+shipping) |
THE BENEFITS OF DIRECT MOXIBUSTION
Moxibustion in general has more or less the same efficacy as acupuncture. However, medical experiments have shown that moxibustion exerts much wider and stronger effect on overall biochemical changes in the body than acupuncture. For example:
(1) It increases the production of white blood cells. The white blood cell count begins to increase immediately after direct moxibustion, and reaches a peak 8 hours later. This peak is maintained for 24 hours. The number remains elevated for four or five days after treatment. The white blood cell count almost doubles with moxibustion, but when applied continuously for six weeks, the increase is sustained for up to even three months after moxibustion is discontinued.
(2) It increases the produciton of red blood cells and haemoglobin. For subjects who had an average haemoglobin ratio of 78% just before direct moxibustion, the ratio increased steadily to reach a peak of 90% in eight weeks. Applying direct moxibustion continuously for 15 weeks, it takes 22 weeks for the red blood cell count to return to what it used to be before moxibustion. It also shows a substantial increase in the following blood components: the sedimentation rate of red blood cells, platelet count, the speed of blood coagulation, blood calcium, blood glucose count and the capacity to produce antibodies.
(3) It improves the overall blood and lymph
circulations. Due to rather intense heat of burning moxa on
acupoints, impulses from nerve endings of the skin cause the dilation of
capillaries
( the smallest vessels) to increase the blood and lymph circulations
in the entire body. In fact it is well known that the patient feels very
warm, relaxed and sleepy from this effect after moxibustion treatment.
People who suffer from constant circulation or "cold feeling" in the hands
and feet can greatly benefit from moxibustion.
(4) It is more effective for internal chronic ailments than acupuncture. Because of stronger effects on the overall biochemical changes, especially in blood components and immune system, moxibustion is much more effective for various chronic diseases of internal organs. From my clinical experiences of over 25 years, I can say that acupuncture can be a better choice for the treatment of rather acute cases or when the ailment is still in early stage.
(5) It is a safer treatment than acupuncture and can be used as a home therapy.
Moxibustion
Moxibustion, or Moxa for short, is an ancient form of heat therapy. Moxa uses the ground up leaves of the plant Mugwort (Artemesia vulgaris). These are either rolled into sticks for indirect moxa, or the powdery substance is made into tiny cones and burned on ointment or a ginger slice. That is called direct moxa. In Chinese, the term for acupuncture is "Zhen Jiu." The "Zhen" means "needle," and the "Jiu" means "moxa." Thus, acupuncture and moxibustion have been paired therapies for hundreds of years.When the needles are in the body, the indirect moxa heats them, and the metal conducts the heat down into the muscles, where it is most needed. However, moxa can be effective by itself, and is an inexpensive form of home therapy for many types of pain, such as sore joints or menstrual cramps.
Burning moxa has a distinct odor, which some people find relaxing. Some people with severe sensitivities to smoke may not be able to tolerate moxa. The essential oils in moxa have a significant effect, as a type of aromatherapy or medicinal incense. All over the world, mugwort has had a good reputation as a plant that keeps evil away. In European folk tradition, mugwort was put into dream pillows to keep bad dreams away. The 'sagebrush' of the west is mostly Artemisia tridentata, closer to mugwort than to sage.
During indirect moxa, the smoldering moxa stick is held a couple inches away from the skin, usually around the inserted needles. The practitioner will monitor the heat level, and work with the patient to provide a therapeutic level of heat while maintaining comfort and safety.
One of the most interesting moxa techniques is for extreme cases of diarrhea. For this, the acupuncturist puts salt in the navel of the supine patient, and puts a cone of direct moxa on top of this. The salt protects the skin and conducts the heat well. This technique is very effective; it seems to regulate the large intestine's resorption of water immediately.
Moxibustion takes skill and caution. It is equivalent to holding a red-hot coal an inch above someone's skin. One needs to exhibit great care when removing the ashes from the end of the stick--if too much force is used while tapping the stick into an ashtray, the "cherry" of the moxa stick may become loose and fall out. Depending on the moxa technique, one may want to let the heat build up as much as the patient can tolerate. When the body's pain threshold is reached, this sends a signal to the body to send more attention to the area being treated: anti-inflammatory compounds, white blood cells, endorphins, etc. I often say that with acupuncture and moxa, we're just trying to encourage the body to prioritize its healing attention on an area it's been ignoring. In some traditions of moxibustion, blistering or scarring was intentionally induced. While that's still used in some areas, it's fortunately uncommon in America. I once treated a Zen Buddhist monk from Japan who had moxa scars all up and down his back. He still complained of back pain, so the scarring moxa wasn't a complete cure.
Gentle moxa is also effective. One of the most famous preventative moxa therapies is to do indirect moxibustion on Zu San Li (Stomach 36), a point on the lower leg. Zu San Li means "Foot Three Miles" and increases endurance, digestive power, and stimulates the immune system.
I use indirect moxa almost daily in the clinic. Most of my patients love it, as the focussed heat feels wonderful on an area which has been tight, in pain, and lacking circulation for some time. I most commonly use moxa on the lower back, sacrum, shoulders, trapezius, and knees.
With some training and much caution, moxa can be an effective home therapy for joint and muscle pain. Improperly handled moxa can lead to burns or pain, so please seek personal instruction before using moxa at home.
Moxa should not be used on diabetics, as they have reduced
heat tolerance and skin weakness. Moxa has been shown effective at turning
a breech baby using the BL-67 point. Moxa could bring on labor, so extreme
care should be taken when using this technique.
Qi—often loosely referred to as energy, or life force, or vital force, and these are part of qi but not its sum total, as it is a moment in time when energy becomes matter, and therefore a process rather than a measurable substance—has various natural means of movement in the environment and in our bodies. When qi moves smoothly through the body, health is balanced, and a person is free of pain. However, when qi begins to be blocked in its smooth movement, it moves in different directions—nausea is referred to as "rebellious stomach qi" because the stomach qi is naturally supposed to move downward (the path of digesting food).
With chemotherapy, from a TCM perspective, the patient is consuming drugs that are classified as energetically cold. This makess sense from a TCM perspective because cancer is classified as blood heat toxin—in other words, the patient's own body has created a mass (tumor) from blood heat that has reached an extreme (toxic) level. This idea of toxin, by the way, is different than that of the natural health movement. While environmental toxins may contribute to many health problems, a balanced body can move through whatever the environment brings it with health. The Chinese recognized that a longstanding inbalance in the body could create a tumor. So to use energetically cold drugs to counteract this heat makes sense.
However, the stomach is susceptible to cold—simpler ways people can make themselves nauseated by accident is eating too many cold foods too fast (a child getting sick off of ice cream, for example). So nausea as a result of chemotherapy points the acupuncturist to two things: open the pathways that the qi is flowing 'backwards' (rebelling) so that it moves down, tonify (support) the stomach, and if the patient normally complains of cold symptoms (getting chilled easily, cold hands and feet, etc.) warm them.
The main acupuncture points to open the extraordinary meridian that courses up the midline of the body and branches out across the chest, the Chong Mai (penetrating meridian) are Pericardium 6 (located two proporational inches up from the wrist between the tendons, over the median nerve—the median nerve is NOT to be stimulated by the needle, this creates hand numbness) and Spleen 4 (located just inferior to the head of the first metatarsal bone of the foot, along the arch of the foot).
A secondary point, which also has the effect of relieving fatigue, stimulating appetite, and strengthening the immune system is Stomach 36, in the space just lateral to the tibial crest, below the head of the tibia, below the knee. The chinese name, zusanli, means "three more miles" indicating that the point was recognized as essential to producing endurance. It supports the immune system function because it helps the body to make both qi and blood from the food (our primary source of both things throughout life).
Moxibustion (the burning of stick or cone moxa, made from mugwort/artemisia vulgaris and possibly wormwood/artemisia absinthum and sage/salvia) is a technique that warms the body and relieves pain. It can be burned over Stomach 36, or over other points, such as on the abdomen or low back, to add to the warming of the patient's entire body.
Finally, since the acupuncturist treats the entire patient, they treat the body in question, chemotherapy and all. Other points may be selected in addition to these important anti-nausea points to address the patient's constitutional imbalances (a general tendency to fatigue, or to stress, or concurrent menopause, etc.). Pain can also be treated. Dietary recommendations may be offered to deal with nausea (adding ginger in all forms to the diet, since it relieves nausea also; adding cooked rice, which is an easily assimilated food, and so on).
While the patient may not in all cases be entirely free of nausea the
day of or after chemotherapy, the severity of the nausa will be drastically
reduced, the recovery time will be shortened, and the appetite will be
maintaned (so that a patient doesn't begin skipping meals as a result).
Fatigue will be relieved, which also improves the patient's general sense
of well-being and promotes optimism about their course of treatment with
chemotherapy.
ZUSANLI (STOMACH-36)
by Subhuti Dharmananda, Ph.D., Director, Institute for Traditional
Medicine, Portland, Oregon
Zusanli is one of the most frequently used of all acupuncture
points and is certainly the most intensively studied single point treatment
in acumoxa therapy. The
indications for use of this acupuncture point are many, and the claimed
benefits are substantial. Many proposals for acupuncture research
in the West rely upon
complex treatment protocols involving several acupuncture points; single-point
acupuncture research to confirm Chinese reports is rare. If one wishes
to demonstrate
that acupuncture is therapeutically beneficial, and to do so with a
simple treatment that is easily reproduced, needling zusanli seems most
appropriate. While many
acupuncturists would prefer, on the basis of their training, to administer
a more complex treatment, few can deny that the proclaimed benefits of
treating this point,
even alone, are worthy of investigation.


With Dr. Paul, Peterborough NH Dec 13 2011
A very sweet person with tons of young children and families
in the audience.
Dr. Paul delivered over 4000 babies_he said he went into
gynecology medicine so he could deliver babies because
he thought it would be a happy type of career.
|
|
| MX101 | Chinese
Traditional Packed Moxa Rolls - used for indirect moxa heat treatment.
Paper covered rolls are approximately 8.3" x 0.75" in diameter.
|
(+shipping) |
HISTORICAL BACKGROUND
Zusanli is one of the 365 classical acupuncture points, located on the
leg portion of the stomach meridian (see Figure
1). According to the analysis presented in
Grasping the Wind (1) the point has had several names attributed to
it, though most of them include the term sanli. In fact, in traditional
acupuncture texts, such as
the Internal Classic (Nei Jing, ca. 100 B.C.) and the Systematic Classic
of Acupuncture (Jia Yi Jing, 1601 A.D.), the point is usually referred
to simply as
sanli. Most authors agree that, as described in Essential Questions
(Nan Jing, ca. 100 A.D.), sanli refers to the method for locating the point
on the leg: it is three
cun (about three inches, or about 4 finger widths; see
Figure 2) below the knee. More specifically, it is 3 cun
below the Stomach-35 point, dubi, parallel to the bottom
of the knee cap. Although the term li is a standard Chinese distance
measurement that normally corresponds to about one-third mile, the term
sanli is a grander one,
more fitting the naming system used for acupuncture points, than sancun.
It has been suggested that li might also have been selected because it
sounds the same as
the related character li meaning to rectify or regulate; for example,
sanli could secondarily imply regulating the three burners.
Zu refers to foot, indicating that the point is on the
portion of the meridian that runs to the foot: the stomach meridian is
often referred to as the foot yangming
meridian. In fact, there is another acupuncture point, shousanli
(Large Intestine-10) which is located 3 cun below the prominent bone of
the elbow; shou refers to
hand, indicating that the point is on the hand yangming meridian, the
large intestine meridian that runs from the hand along the arm.
One other name for zusanli that is of particular significance
is xiaqihai, meaning lower sea of qi. The upper sea of qi, simply
called qihai (Conception Vessel-6),
is located at the dantian (which is below the navel about 1.5 inches).
The dantian is thought to be the primary reservoir of the body’s qi, at
least according to the
Taoist tradition. One of the key Taoist breathing exercises involves
abdominal
breathing with visualization of air, a type of qi, being drawn to this
spot (“breathing into
the dantian”). In the Ling Shu (2) it is said that “the center
of breathing is the sea of qi.” Thus, the term xiaqihai implies that
needling this point may have an effect
comparable to needling qihai.
In the Nei Jing Su Wen (3), the bilateral zusanli points
are mentioned as two of the eight points for eliminating heat from the
stomach. Zusanli is also mentioned
as a treatment for knee pain that “feels so severe that the tibia feels
broken.” Zusanli is described as a he point (confluence point) of
the stomach meridian. He points
are where the qi submerges in its flow along the meridian; it submerges
into the vast interior ocean of qi and blood. According to Essential
Questions, confluent
points are indicated for treating diarrhea caused by unhealthy qi.
The Ling Shu mentions that confluent points are indicated for disorders
in the fu organs (the
stomach is one of the fu organs). The Systematic Classic of Acupuncture
(19) includes these indications for zusanli:
For cold in the intestines with distention
and fullness, frequent belching, aversion to the smell of food, insufficiency
of the stomach qi, rumbling of the
intestines, pain in the abdomen, diarrhea
of untransformed food in the stools, and distention in the region below
the hearts, sanli is the ruling point.
In a collection of odes to acupuncture (20), also obtained
from the Systematic Classic of Acupuncture, the following statements about
zusanli are made:
·
Acute diarrhea and vomiting, search out yingu (Kidney-10) and sanli (Stomach-36).
·
Who knows in a weakening cough to search instantly for sanli?
·
A sound like cicadas in the ear which you want to diminish, be certain
to keep in store the point sanli below the knee.
·
A little boy with indigestion, sanli is noblest.
·
If perhaps the bladder does not disperse water, then again it is suitable
to seek within sanli.
·
If there is dizziness as you plunge the needle in [while performing acupuncture],
immediately reinforce zusanli or reinforce renzhong (Governing Vessel-26).
·
If the mind is perturbed and anxious, pierce sanli.
·
Sanli removes great debility arising from malnutrition—Hua Tuo mentioned
this.
·
Cold and numbness when the kidney qi is shriveling—select the earth point
of foot yangming [zusanli]
·
Heal a breath blocked above with zusanli.
A more lengthy discourse on the value of this point is
included (20) in “Ma Danyang’s song on the twelve points shining bright
as the starry sky and able to heal all
the many diseases”:
Sanli under the eye of the knee, three cun,
in between the two tendons, one can reach into the center of a swollen
belly, it is splendid at healing a cold
stomach, intestinal noises, and diarrhea,
a swollen leg, sore knee, or calf; an injury from cold, weakness or emaciation,
and parasitic infection of all sorts;
when your age has passed thirty, needle and
moxa at this point; change your thinking to find it, look extremely carefully;
three cones of moxa, eight fen in,
and peace.
There are also references in the book to using zusanli
along with other points to treat beriberi (this medical term refers to
swelling of the legs that is due to vitamin
B1 deficiency, a common problem in the Orient; obviously, the original
statement did not specify the cause of the leg swelling). In addition,
there is an explanation of
why needling zusanli during pregnancy is contraindicated, except at
the time of delivery:
At one time in the past, the Song Dynasty
Crown Prince loved the medical arts. He was out wandering in his
park when he came across someone
looking after a pregnant woman. The
Crown Prince made a diagnosis on her and said: “The baby is a girl.”
He ordered the physician Xu Wenbai to
make a diagnosis; Wenbai replied: “There are
twins, a boy and a girl.” The Crown Prince was furious and wanted
to cut the woman’s belly open to find
out. Wenbai stopped him, saying: “please
may I use my humble needles?” The he drained zusanli, and reinforced
hegu (Large Intestine-4), and the
fetuses responded to his needle and fell.
And it turned out to be as Wenbai had predicted. Therefore, it is
now said one should not needle these points on
pregnant women.
MODERN INDICATIONS
The current standard indications for zusanli, as reviewed in Advanced
Textbook of Traditional Chinese Medicine and Pharmacology (21) are: stomach
ache,
abdominal distention, vomiting, diarrhea, dysentery, indigestion, appendicitis,
flaccidity and numbness of the lower limbs, edema, mastitis, mania, epilepsy,
cough, vertigo,
palpitation, and emaciation due to consumptive disease. This
latter indication corresponds to the concept that needling this point can
tonify the sea of qi and thereby
help to stop the wasting disease and restore ones body weight and vitality.
To illustrate the uniformity of indications amongst the
Chinese authorities, the following were listed in Chinese Acupuncture and
Moxibustion (22, 23), with
slight differences on translation between the original Chinese and
later Western publications: gastric pain, hiccup, abdominal distention,
vomiting, diarrhea, dysentery,
emaciation due to general deficiency, constipation, mastitis, intestinal
abscess (acute appendicitis), numbness (motor impairment) and pain of the
lower extremities,
edema (beriberi), manic depressive psychosis.
In another book by the same name, Chinese Acupuncture
and Moxibustion (24), these are listed: gastric pain, vomiting, hiccup,
abdominal distention,
borborygmus, diarrhea, dysentery, constipation, mastitis, enteritis,
aching of the knee joint and leg, beriberi, edema, cough, asthma, emaciation
due to general deficiency,
indigestion, apoplexy, hemiplegia, dizziness, insomnia, mania.
As these indications may suggest, zusanli is often applied
in emergency situations. In a report on emergency acupuncture (25),
Zhang Xiaoping mentioned use of
zusanli, accompanied by other points, for treating high fever, syncope,
pulmonary abscess (with expectoration of sticky, foul, or bloody sputum),
sudden vomiting,
sudden diarrhea, fulminant dysentery, acute jaundice, acute hypochondriac
pain, acute epigastralgia, acute abdominal pain, acute stranguria, sudden
swelling (acute
edema), and dysuria with vomiting (usually due to renal failure).
CLINICAL RESEARCH
There have been two main directions taken in modern clinical research
with treatment at zusanli. One is the treatment of abdominal pain
and spasm, usually affecting
the stomach, gallbladder, or kidney. In this case, stimulation
of the acupuncture point is reported to have immediate effects (within
seconds or minutes) and patients
often receive only one treatment. These reports are presented
first. The other is the treatment of impaired immune functions, especially
deficits in leukocyte and
immunoglobulin production. In this case, stimulation of the acupuncture
point is carried out daily, usually for 10–14 days consecutively, and this
course of therapy might
be repeated (sometimes after a short break of a few days). One
of the studies mentioned below combines these two areas of concern: treatment
of cancer patients
suffering from abdominal pain (cancer patients usually have impaired
immune functions, either spontaneously or as the result of medical therapies).
As might be expected, the relationship of zusanli to stomach
function has been one of the main aims of research into the action of acupuncture
stimulus applied at
this point. It has been reported generally that needling zusanli
can strengthen the contraction and digestive function of the weak stomach
and relax the spasms of the
stressed stomach. This latter indication has been investigated
directly.
For example, in the 1984 Journal of Traditional Chinese
Medicine (4), a group at the Gastroenterology Section of the hospital affiliated
with Guiyang College of
Traditional Chinese Medicine published a report on needling zusanli
while administering the fiberoptic gastroscopy test. This test, in
which a fiber optics tube is
inserted through the mouth, down the throat, and into the stomach and
then into the duodenum, tends to cause gastric and pyloric spasms.
The authors of the study,
relying on previous laboratory animal and clinical acupuncture investigations,
believed that needling zusanli would be a reasonable treatment for the
induced gastric
spasms. In the article’s discussion they said that “No few recent
studies indicate that zusanli needling has a regulatory effect on gastrointestinal
tract function.”
Their patients were treated by standard Western medical
methods that included premedication with atropine sulfate and valium; but
about 10% of their patients
suffered from persisting gastric or pyloric spasm, and these patients
were treated by needling zusanli on the right side (the patients were lying
on their left side during
the gastroscopy procedure, making the right leg more accessible).
The needle technique was to use rapid insertion, an insertion depth of
3.5–4.0 centimeters (about
1.5 cun), and an insertion angle towards the abdomen. The needle
was twisted and rotated with “moderate stimulation,” until a propagated
sensation from the treated
point to the abdomen was felt. The needle was retained until
the examination was over. According to the authors, this treatment
relieved the spasms of 59 of the 60
patients so treated. The duration of needling required to get
relief was within a few seconds in 9 cases, one minute in 13 cases, 2 minutes
in 13 cases, 3 minutes in 12
cases, and 5 minutes in 12 cases.
A similar study was reported in the 1987 Journal of Traditional
Chinese Medicine (5). In this case, the authors, from the China Medical
University affiliated
hospital, treated the control group with atropine and valium, but not
the acupuncture group, who were treated, instead, at zusanli. The
point hegu (Large Intestine-4)
was also needled. As with the other study, patients were lying
on their left side and acupuncture was administered only on the right side.
Electroacupuncture was utilized after obtaining the qi
reaction by manual stimulation. The electric stimulus, at 2.5 Hz,
was administered for 10–15 minutes prior to
beginning gastroscopy. The needles were withdrawn after the gastroscopy
was completed. The authors reported that 68 out of 70 patients had
satisfactory
introduction of the gastroscope; it worked as well as the drug therapy.
Further, while patients in the control group reported some dizziness and
malaise after treatment
(probably due to the drug effects), this was not reported in the acupuncture
group.
Along somewhat similar lines, elderly patients with epigastric
pain were recruited for a study of zusanli at the Wuhan Hospital of Traditional
Chinese Medicine,
reported in the 1992 Journal of Traditional Chinese Medicine (6).
The author pointed out that this pain syndrome usually arises from stagnation
(which is a type of
excess) on a background of overall deficiency, and that zusanli is
an ideal point because it can alleviate the gastrointestinal local disorder
while providing tonification.
Zusanli was punctured to a depth of 1.5 cun, followed
by twisting and thrusting the needle to attain the propagated qi reaction
(soreness and distension that radiates
to the epigastrum). The needle is retained for 10–20 minutes,
during which time it is maneuvered 1–2 times in cases of severe pain.
The author presented three
sample cases of successful treatment: two with billiary pain and one
with stomach pain. According to the reports, the pain would be alleviated
within 10–20 minutes of
beginning the treatment.
A short report on needling zusanli to alleviate renal
colic, which, in China, is usually treated with atropine or dolantin, appeared
in the 1993 Journal of Traditional
Chinese Medicine (7). The author needled patients bilaterally
at zusanli with a needle depth of 2–2.5 cun (which is deeper needling than
usual), with rapid twisting and
rotation for strong stimulation for 1–2 minutes. The pain was
reported to be alleviated promptly. The same treatment would be given
again if the pain returned, in
place of using injection of drugs.
An extensive review of using zusanli in abdominal surgical
applications and abdominal pain, alone or as the main point in an acupuncture
treatment, was presented
recently by Cui Yunmeng and Qi Lijie (35). Among the applications
and findings (outcome details not included here) were these:
· Acute
appendicitis: patients would first be treated at zusanli with strong stimulation
applied for 3–5 minutes after getting the qi reaction; if the abdominal
pain
was obviously reduced, the patient would
then be treated by non-surgical methods, mainly by additional acupuncture
applied at zusanli; if the pain could not be
reduced, the patient was treated surgically.
· Post-operative
pain: patients could be treated by injection at zusanli. According
to the report, injection of vitamin K3 at this point, but not intramuscularly
elsewhere, would provide pain relief
for all patients; injecting water at the point brought pain relief to 73%
of those treated. Referring to previous research, the
author mentioned that needling zusanli
could raise the pain threshold and inhibit pain transmission in the nervous
system, especially in the abdominal area.
· Acute
abdominal pain from various causes: electro-acupuncture at zusanli was
used to treat pain due to acute pancreatitis, appendicitis, biliary ascariasis,
renal
and urethral calculus, and adhesive
intestinal obstruction. Treatment provided prompt pain relief; and
recurrence of pain within 24 hours was only 30% in those
receiving acupuncture at this point.
Differential treatment (using various acupuncture points according to standard
Chinese medical diagnostic categories) did
not improve the outcomes.
Although abdominal pain is the main focus of treatment
with zusanli, the point is also used for leg pain and for temporomandibular
joint pain. The latter application
comes about because the stomach meridian runs along the face, crossing
the temporomandibular joint (see Figure 3).
A report by Cui Yunmeng (30), detailed the
results of treating 60 patients with temporomandibular joint pain,
difficulty opening the mouth, and problems with mastication. The
author used single point
acupuncture, stimulating zusanli only on the side of the body corresponding
to the side of the face that was affected. The needle was stimulated
to get the qi reaction,
with an insertion depth of 1 cun, retaining the needle for 20–30 minutes.
Patients received just 1–6 treatments, typically 3–4 treatments.
According to the author, 39
patients were cured, and 15 cases were markedly improved; the other
6 showed minor improvement. Cui also reported (35) treating chest
pain in the area of the
mammary gland caused by soft-tissue injury, intercostal neuralgia,
and acute mastitis, needling zusanli only on the same side as that affected
by pain. As with the
facial pain, the rationale for using zusanli for chest pain was that
the stomach meridian runs upward across the ribs, through the mammary area.
The treatment of abdominal pain by needling zusanli was
investigated in cancer patients at the affiliated cancer hospital of Harbin
Medical University, reported in
the 1995 Journal of Traditional Chinese Medicine (28). The patients
were not getting relief from standard pain medication. The cancer
cases included liver cancer,
post-surgical stomach cancer, recurrent colon cancer, and abdominal
lymphosarcoma.
Zusanli was treated on both sides, using either the reinforcing
or reducing stimulation technique, depending on the traditional diagnosis
of the patients. After
attaining the needling sensation, the needles were retained for 15
minutes. Acupuncture was administered daily for two weeks as a course
of therapy. In all but 11 of
the 92 cases so treated, there was some degree of pain relief.
Minor pain was alleviated in all cases, but more severe pain was usually
only partially remitted. Still, in
the group rated as having moderate pain, one-third attained pain relief
that persisted for one month or more. The authors reported that there
was pain relief during the
needling session, and that persisting results could be attained after
several consecutive days of treatment (typically, the full 2 weeks).
They summarized the ability of
the single point treatment to alleviate the cancer pain as follows:
“If the duration [of suffering from cancer pain] is short, pain grade is
low, tumors are small in size
with no or little metastasis, the effect [of acupuncture at zusanli]
is good....Also, the effect is related to the mental state of the patients.
If they are full of confidence
and cooperative in the treatment, better results can be expected.”
The authors cited earlier research (1989) that purported
to show that needling zusanli could inhibit the nerves that cause the condition
known as qi counterflow,
which often causes spasms and vomiting. They also cited earlier
research (1987 and 1990) with laboratory animal studies revealing that
the corresponding zusanli
point on animals yielded significant analgesic effects. Finally,
they suggested that needling zusanli could have an anticancer activity
(thus alleviating pain by reducing
the impact of the cancer), because earlier research (1989) had shown
that needling this point could increase the number of T-cells and improve
the activity of natural
killer cells.
The immunological action of needling zusanli has been
the subject of some clinical research. For example, a group or researchers
at the Zhong Guan Cun Hospital
in Beijing and members of the Chinese Academy of Traditional Chinese
Medicine (9) reported on the effects of stimulating zusanli with laser
radiation or heat
(provided with a focused flashing light source that measurably raised
the skin temperature). They stimulated the bilateral zusanli points
by either of these methods for
10 minutes at a session, once daily for 14 consecutive days.
According to their report, healthy elderly individuals (60–77 years) treated
by either method showed
significant increases in peripheral blood leukocytes and total immunoglobulins.
A study exploring the ability of needling at zusanli to
treat leukopenia was reported in a recent issue of the 1998 Journal of
Traditional Chinese Medicine (10). In
this case, leukopenia from various causes, mainly unknown etiology,
with some cases from side effects of drugs and radiation or secondary effects
of advanced
diseases, was treated with acupuncture in 14 days of consecutive sessions.
After a one week break, another 14 days of consecutive sessions was applied.
The
needles were inserted to zusanli on both legs, at a depth of about
1 cun. With twirling and lift-and-thrust maneuvers, the qi reaction
was attained (soreness and
distension), and then the needle was retained for 20 minutes with manipulations
every 5 minutes. According to the report, there were significant
improvements in
immunoglobulin levels (IgG, IgA, and IgM; though IgG, which causes
joint inflammation in arthritis patients was reported to be reduced in
2 patients of this group who
had advanced arthritis), in C3 (complement protein 3), and in phytohemagglutinin
test. According to the author:
Zusanli is a point for recuperating the depleted
yang, and also one of the important points for strengthening the body resistance.
Its action in health
preservation has been paid due attention by
doctors of successive dynasties....Acupuncture at zusanli can enhance both
the specific and non-specific
immunological function of the body.
Interestingly, although zusanli has been described in
the past as treating cold conditions of the stomach (but, in the Nei Jing
it is indicated for stomach heat), it is
not usually depicted in the traditional literature as recuperating
depleted yang. The one exception cited in the historical review
above is the statement in the Jia Yi
Jing that one could stimulate zusanli to treat “cold and numbness when
the kidney qi is shriveling.” Rather, the point is frequently said
to “regulate qi and blood.”
Nonetheless, the depiction of zusanli invigorating the yang, which
is not specifically mentioned in the modern acupuncture textbooks, is relied
upon clinically in the
treatment of impotence (zusanli is combined with a few other points).
While one can say that anything that improves body function strengthens
resistance to
pathological influences (in the case quoted above, specifically to
infections, since immunological function is then described), the traditional
literature does not appear to
emphasize this action. The author’s statement thus reveals how
Chinese researchers can skew the explanation of what has been done in past
dynastic periods to fit
their particular findings.
ACUPUNCTURE MECHANISMS RESEARCH
Because of the importance attributed to zusanli in modern times, it
has been a point commonly tested in evaluations of how acupuncture might
work. That is, in
attempting to find modern medical descriptions for the functions of
acupoint stimulation, various responses of laboratory animals are determined.
Zusanli on animals is
located on the lateral tibial prominence, 1/5 of the distance from
the knee to the ankle (11). This method of finding the point corresponds
to the human measurement
system, in which the distance from the knee to the ankle is said to
be 16 cun (zusanli, at 3 cun, is thus about 1/5 the distance).
One suggestion about how acupuncture functions is that
nerves are stimulated at the point (this yields the qi reaction as the
sensory aspect, but can also involve
non-sensory signals), and signals transferred along nerve pathways
yield the ultimate therapeutic effect. There are two possibilities
that may be considered:
1. The nervous system transfers signals
directly from the acupoint to the organ that is being treated. The
importance Chinese doctors attach to obtaining a
propagated qi sensation along this pathway would imply
this mechanism is involved.
2. The nervous system transfers information
to the brain first, which then yields the response that affects the target
area.
Both of these mechanisms could be involved in the total
effect, along with release of substances from the nervous system into the
blood stream during the
transmission of signals. The released substances could interact
with the endocrine and immune systems to generate systemic effects.
As Cai Wuying concluded in his
article on acupuncture and the nervous system (33): “Acupuncture stimulates
peripheral sensory nerves and their endings, increases cutaneous blood
flow and
microcirculation, and releases neurotransmitters, neuropeptides, and
hormones.”
To test the involvement of the nervous system, laboratory
animal experiments were utilized in which nerves in the legs of animals
were severed and it was shown
that the effects of needling the point equivalent to zusanli could
be stopped (23). Other experiments indicated that by blocking the
nerve trunks related to the
acupuncture points with procaine, the increase in white blood cell
counts that are accomplished by stimulating zusanli (usually along with
other points) is also blocked.
This would suggest that nerve transmission is, in fact, an important
part of the full range of therapeutic functions.
In the case of epilepsy, a laboratory animal experiment
was reported in the 1992 Journal of Traditional Chinese Medicine (12),
with needling at zusanli. The
authors concluded that: “All the observations lead to the presumption
that electroacupuncture when applied at zusanli exerts seizure-suppressing
effect through a
pathway of hypothalamic arcuate nucleus to brain stem raphe nucleus,
to hippocampus.” The pathway leading from the acupuncture point to
the brain stimulation,
which released neurotransmitters to affect the other parts of the brain,
was not investigated in this study, but a transmission via nerves is certainly
a reasonable
explanation. This is especially so since the effects on the brain
were immediate: showing up shortly after the electro-acupuncture was started
and diminishing when
acupuncture therapy was stopped. The transmission from the acupuncture
points were depicted in another study (26) this way: “the afferent impulses
from the
acupuncture points may activate the enkephalinergic neurons in the
periaqueductral gray matter, especially in the dorsal part, and trigger
the release of opiate-like
substance which in turn acts on the nucleus raphe magnus.” The
afferent impulses refer to nerve transmissions from the acupuncture site
to the brain. In this study,
bilateral zusanli were the points selected for stimulation.
Another study of zusanli on the brain was conducted in
rabbits (29), in which it was shown that stimulating the zusanli point
markedly increased blood flow in the
cerebral tissues. The effect could be seen immediately after
the stimulation began (first measurement one minute after initiating needle
stimulus), and it increased
during the next several minutes). The authors compared the effects
of electroacupuncture stimulation with manual twirling manipulation of
the needle using either the
reducing or the reinforcing method. They reported that electroacupuncture
had a much greater effect on the cerebral blood flow, while the two manual
methods
produced a lesser effect of the same nature, with no evident difference
between the results of reducing or reinforcing methods. Presumably,
the change in blood flow,
which has also been reported to be a result of scalp acupuncture (see:
Synopsis of scalp acupuncture), is accompanied by changes in brain activity.
In a study of immunological effects of needling zusanli
mentioned in a review article (13), it was reported that the total white
blood cell count of rats and rabbits
could be increased markedly by needling zusanli, reaching a peak value
with five consecutive days of treatment. However, this effect could
only be achieved when
the nervous and adrenal systems were intact. Aside from white blood
cell counts, several other beneficial immunological effects of needling
or moxibustion application
at zusanli, either alone or in combination with other points, were
mentioned in the review article.
In a study of hormonal effects, electro-acupuncture at
zusanli was administered to dogs who had impaired adrenocortical function
after three weeks administration
of prednisone (34). Zusanli was treated bilaterally for 30 minutes,
three times per week, for three weeks. Control animals received a
similar stimulus either at points
on the bladder meridian close to the adrenal glands (BL-22, -23, and
24) or at a non-acupuncture point. According to the report,
ACTH was markedly improved
during acupuncture therapy at zusanli, was only slight improved by
acupuncture on the bladder meridian points, and not affected by treatment
at the non-acupuncture
point. Serum cortisol markedly improved in the zusanli group
during the three week course of therapy. The authors pointed out
previous research indicating that
needling zusanli in several animal models (rabbits, cows, and sheep)
could increase plasma hormones, and that the adrenocortical hormones were
being stimulated via
the hypothalamus (which is encompassed by the brain). An effect
of acupuncture on the higher brain center was suggested as a possible basis
for the
hypothalamic-adrenal response.
It is not clear that such mechanistic explanations contribute
very much to the actual clinical practice of acupuncture, though they do
lend support to the Chinese
contention that attaining the qi reaction and, in some cases, the propagated
qi sensation, may be critical to attaining success in the treatment (see:
Getting Qi). These
reactions are felt by the patient and obviously represent successful
interaction with the nervous system.
For example, in a study reported in 1989 Journal of Traditional
Chinese Medicine (14), in which asthma patients were treated at acupuncture
points zusanli and two
lung points (taiyuan and chize, Lung-9 and Lung-5), it was found that
the patients experiencing a strong propagated needle sensation got good
results, while those who
experienced little of this sensation had poorer results. In the
case of zusanli, the direction of propagation was downward; for chize,
it was mainly upward, with 20% of
patients reporting radiation in both directions. The authors
commented:
Whether or not acupuncture produces needling
sensations bears a close relationship to the therapeutic results.
Centuries ago, it was pointed out in the
Nei Jing that the results of treatment can
be obtained only when needling sensation reaches the site of disease....During
acupuncture, the doctor’s
attention should be given to needle manipulation
in order to elicit adequately strong sensations. Strong sensations
not only lead to more ideal results but
also improve the objective indicies....”
SIMPLE COMBINATIONS WITH ZUSANLI
Because zusanli is so widely used by acupuncturists, it is naturally
included in combinations with numerous other points. Certain combinations
appear with especially
high frequency. Below are some examples of treatments that specifically
involve a small number of points. Probably the most frequent combination
is with hegu
(Large Intestine-4). This combination was mentioned in the story
about inducing childbirth and in one of the gastroscopy trials, and is
also described in some of the
acupuncture mechanism experiments. In Modern Clinical Necessities
for Acupuncture (15), treatment of this combination of points is cited
as a successful
treatment for the new application of giving up smoking.
In a study on the immunological effects of acupuncture
(16), 120 patients suffering from pain syndromes were treated with acupuncture
at zusanli and hegu. The
researchers selected these points because:
For years, Chinese authors described that
acupuncture can have a stimulating effect on cell-mediated immunity.
In fact, some experimental research
suggests a fairly good increase of T-lymphocytes
after acupuncture stimulation at zusanli and hegu acupoints, as well as
an increase of lymphoblast
transformation which persists for 24 hours
after stimulation.
Treatment was carried out with perpendicular insertion
of the needles, with varying depth depending on the patients constitution
(range: 0.8–3.3 cm). Twisting and
twirling manipulation of the needles was used to attain the qi reaction.
Stimulation was continued, with one minute of stimulation at a time, bilaterally,
for each point,
with a one minute break between stimulus sessions. After 15 minutes,
stimulation of hegu continued by the same method, but zusanli was stimulated
by electrical
apparatus at 90 Hz. The needles were withdrawn after 30 minutes.
According to the authors, 77% of the treated patients showed an increase
in CD3 and CD4 cells
30 minutes after completion of the acupuncture treatments. Based
on analysis of immune changes over time, the authors concluded that antibody-dependent
cell
cytotoxicity by monocytes was strengthened, which is important for
treating infectious diseases. Also, natural killer cells were stimulated
by the acupuncture; these
yield cytotoxic activity against virally infected cells and cancer
cells. The authors believed that their results, which included analysis
of vasoactive intestinal peptide
(VIP) and endorphins, confirm the recent findings with regard to neuroimmunomodulation
(the regulation of the immune system via the nervous system).
Other common pairings:
· Zusanli
and neiguan (Pericardium-6). These two points were the primary ones
used in a study of cancer therapy (8), though others were sometimes added
for specific symptoms. It was
claimed that the acupuncture treatment ameliorated the typical side effects
of chemotherapy and radiation therapy (poor
appetite, nausea, vomiting, diarrhea,
dizziness, insomnia, and fatigue) and improved the immune functions (including
leukocyte count and immunoglobulin
levels). In a review article on
acupuncture research (32), Kuang Yihuang and Wei Jia made reference to
research published in 1981: “Not a few patients
suffering from drug intoxication and
allergy [reaction to drugs] have been treated by acumoxibustion.
Reactions such as vomiting, arthralgia, involuntary
muscle movements, tachycardia, proxysmal
chronic bronchitis and hypertension from antimony artrate injection and
T273 administration have been cured by
needling zusanli and neiguan bilaterally
for 10–13 sessions.”
· Zusanli
and sanyinjiao (Spleen-6). In a study of cancer patients receiving
radiation therapy (17), patients were treated with microwave stimulated
acupuncture at zusanli and sanyinjiao.
The needles were inserted to 1.5 cun depth, and manipulated by hand to
attain the qi reaction. The needles were then
attached to microwave stimulus to maintain
a needling sensation. Treatment time was 20 minutes each day, for
10 consecutive days. Leukocyte levels, which
had been lowered by the radiation therapy,
were monitored. According to the report, this acupuncture therapy
was more effective in raising leukocytes than
Western drugs (including leucogen) given
to a control group. Further, the acupuncture group started with greater
impairment of leukocytes. In another study,
the same two points were reported to
aid recovery of movement in the intestines following abdominal surgery
and to lower liver enzyme levels that were
raised as the result of tissue damage
during surgery (35).
The four acupuncture points mentioned here, zusanli, hegu,
neiguan, and sanyinjiao, were used together as the main points in a study
involving the treatment of
pain due to stomach cancer (31). Needle stimulus was carried
out by reinforcing or reducing method and needles were retained for 20
minutes. The patients were
asked to concentrate their minds on the diseased part (the stomach)
during the treatment. Acupuncture was given daily for 14 days; after
a break of 2–3 days another
course of 14 days treatment was given for a total of 4 courses of therapy
lasting two months. The authors reported that 80% of patients experienced
immediate
analgesic effects; about half of those patients maintained good analgesic
effects 12 hours after the treatment. After two months of regular
treatment, over 90% of the
patients attained good analgesic effects. Among a control group
receiving Western medications for pain (including codeine and dolantin,
prescribed as needed), the
immediate effects of the drugs were superior to acupuncture analgesia,
but after two months of therapy, the acupuncture effects were as good as
the drug effects.
The authors also monitored the effects of their treatments on the immune
system, on chemotherapy side effects, and quality of life, indicating that
acupuncture had
notable benefits not matched by the Western medicine group.
Previous reports have shown similar responses to treatment
at zusanli alone, so it remains unclear whether the more complex therapy
used in this study was really
necessary. Needling several points with adequate stimulus is
more complicated for the practitioner and is more confusing for the patient
who is asked to focus his or
her mind on the diseased part.
There are also some needle groupings that are larger but
have become somewhat standard practice and involve zusanli. For example,
Miriam Lee, in her book,
Insights of a Senior Acupuncturist (18), describes the combination
of “antique points,” sometimes called “ten old needles,” which is comprised
of bilateral
acupuncture at five sites, including three of the sites mentioned above:
zusanli (Stomach-36)
hegu (Large Intestine-4)
sanyinjiao (Spleen-6)
quchi (Large Intestine-11)
lieque (Lung-7)
This combination is used for a wide range of disorders.
Regarding zusanli, Lee reports:
It increases digestion, helps the body to
absorb food, increases the production of gastric acids, and stimulates
hunger. I needle it first because it
tranquilizes the patient and protects them
from fainting reaction to the needles. It increases the flow of energy
and oxygen to the head, since the stomach
channel begins on the head. When needling
the stomach channel on the feet, all the qi is sent upward. After
stimulating zusanli, you can see the face
become infused with redness, glowing and warm.
Technique is very important. I put in both needles and then de qi
(obtain the qi). Then with my right
hand on the needle in the left leg and my
left hand on the needle in the right leg, with the needles inserted shallowly,
I move both thumbs forward 240
degrees and backwards 120 degrees (2/3 of
a full turn around forward and 1/3 turn back). This is done 3 times
and then the needle is thrust a little
deeper, turned as above 3 times, again thrust
deeper and turned 3 times, for a total of 9 turns. It is important
that both needles be turned at the same
time....Repeat the turnings 9 times until
the propagation of qi reaches the toes....After the qi has reached the
end of the channel, pull the needle up above
the channel and above the muscle but not out
of the skin and leave it shallow, pointing in the direction the channel
flows. In the case of the stomach
channel, point it towards the foot.
This is the technique for supplementation.
Although Lee emphasizes a particular stimulation technique,
the previously mentioned research appears to demonstrate effective response
to other methods of
stimulation.
A similar approach was used by Wang Leting (27), a well-known
acupuncturist in China who practiced there from 1929 to 1979. Regarding
zusanli, he is reported
to have said “For hundreds of diseases, don’t forget zusanli.”
In his records of treatment for gastro-intestinal diseases, it was found
that he had used zusanli more
often than any other point, in 72% of 126 cases treated. His
own formula for ten old needles was:
zusanli (Stomach-36)
zhongwan (Conception Vessel-12)
qihai (Conception Vessel-6)
tianshu (Stomach-25)
neiguan (Pericardium-6)
Although this differs markedly from the one mentioned
by Miriam Lee, he had a similar formulation which he referred to as Shiquan
Dabu Tang acupuncture.
Shiquan Dabu Tang (Ginseng and Tang-kuei Ten Combination), is a qi
tonifying and blood nourishing herbal formula that has numerous uses, including
counteracting
adverse effects to Western medical therapies. His formula is
the same as Lee’s, except that liqie (Lung-7) is deleted and replaced by
a combination five points:
lingquan (Gallbladder-34), zhongwan (Conception Vessel-12), taichong
(Liver-3), zhangmen (Liver-13), and guanyuan (Conception Vessel-4).
He recommended
this set for the treatment of spleen-heart deficiency, spleen-kidney
deficiency, and liver-kidney deficiency syndromes.
REFERENCES
1. Ellis A, Wiseman N, and Boss K, Grasping
the Wind, 1989 Paradigm Publications, Brookline, MA.
2. Wu Jing-Nuan (translator), Ling Shu,
or The Spiritual Pivot, 1993 Taoist Center, Washington, D.C.
3. Maoshing Ni, The Yellow Emperor’s
Classic of Medicine: A New Translation of the Neijing Suwen with Commentary,
1995 Shambhala, Boston, MA.
4. Cheng Yiqin, et al., The use of needling
zusanli in fiberoptic gastroscopy, Journal of Traditional Chinese Medicine
1984; 4(2): 91–92.
5. Chu Hang, Zhao Shuzhen, and Huang
Yuying, Application of acupuncture to gastroscopy using a fiberoptic endoscope,
Journal of Traditional Chinese
Medicine 1987; 7(4): 279.
6. Zhang Jueren, Treatment with acupuncture
at zusanli for epigastric pain in the elderly, Journal of Traditional Chinese
Medicine 1992; 12(3): 178–179.
7. Liu Guoliang, Treatment of renal colic
with acupuncture at zusanli, Journal of Traditional Chinese Medicine 1993;
13 (4): 265.
8. Xia Yuqing, et al., An approach to
the effect on tumors of acupuncture in combination with radiotherapy or
chemotherapy, Journal of Traditional Chinese
Medicine 1986; 6 (a): 23–26.
9. Peng Yue, et al., Effects of laser
radiation and photobustion over zusanli on the blood immunoglobulin and
lymphocyte ANAE of the healthy aged,
Journal of Traditional Chinese Medicine 1987; 7(2): 135–136.
10. Wei Zanmei, Clinical observation on therapeutic effect of
acupuncture on zusanli for leukopenia, Journal of Traditional Chinese Medicine
1998; 18(2):
94–95.
11. Hua Xingbang, On animal acupoints, Journal of Traditional
Chinese Medicine 1987; 7(4): 301–304.
12. Wu Dingzong, Mechanism of acupuncture in suppressing epileptic
seizures, Journal of Traditional Chinese Medicine 1992; 12(3): 187–192.
13. Cui Meng, Present status of research abroad concerning the
effect of acupuncture and moxibustion on immunological functions, Journal
of Traditional
Chinese Medicine 1992; 12(3): 211–219.
14. Sheng Lingling, et al., Effect of needling sensation reaching
the site of disease on the results of acupuncture treatment of bronchial
asthma, Journal of
Traditional Chinese Medicine 1989; 9(2): 140–143.
15. Wang Qi and Dong Zhi Lin, Modern Clinical Necessities for
Traditional Chinese Medicine, 1990 China Ocean Press, Beijing.
16. Petti F, et al., Effects of acupuncture on immune response
related to opioid-like peptides, Journal of Traditional Chinese Medicine
1998; 18(1): 55–63.
17. He Chengjiang, Gong Kehui, and Xu Qunzhu, Effects of microwave
acupuncture on the immunological function of cancer patients, Journal of
Traditional
Chinese Medicine 1987; 7(1): 9–11.
18. Lee M, Insights of a Senior Acupuncturist, 1992 Blue Poppy
Press, Inc., Boulder, CO.
19. Huang-fu Mi, Systematic Classic of Acupuncture and Moxibustion,
1994 Blue Poppy Press, Inc., Boulder, CO.
20. Bertschinger R (translator), The Golden Needle, 1991 Churchill
Livingstone, London.
21. Ming Shunpei and Yang Shunyi, Advanced Textbook of Traditional
Chinese Medicine and Pharmacology, Volume 4 1997 New World Press Beijing.
22. Zhang Enquin (Ed. in Chief), Chinese Acupuncture and Moxibustion,
1990 Publishing House of Shanghai College of Traditional Chinese Medicine.
23. Qiu Mao-liang (Man. Ed.), Chinese Acupuncture and Moxibustion,
1993 Churchill Livingstone, London.
24. Chang Xinnang (Chief Ed.) Chinese Acupuncture and Moxibustion,
1987 Foreign Language Press, Beijing.
25. Zhang Xiaoping, Indications and contra-indications in emergency
acupuncture treatment, Journal of Traditional Chinese Medicine 1996; 16(1):
70–77.
26. Zhu Lixia and Shi Qingyao, Activation of nucleus raphe magnus
by acupuncture and enkephalinergic mechanism, Journal of Traditional Chinese
Medicine
1984; 4(2): 111–118.
27. Yu Hui-cha and Han Fu-ru, (Shuai Xue-zhang, Trans.), Golden
Needle Wang Le-ting, 1996 Blue Poppy Press, Inc., Boulder, CO.
28. Xu Shuying, Liu Zhiqiang, and Liyu, Treatment of cancerous
abdominal pain by acupuncture on zusanli, Journal of Traditional Chinese
Medicine 1995; 15(3):
189–191.
29. Shi Renhua, et al., Effects of electroacupuncture and twirling
reinforcing-reducing manipulations on volume of microcirculatory blood
flow in cerebral
pia mater, Journal of Traditional Chinese Medicine 1998;
18(3): 220–224.
30. Cui Yunmeng, Treatment of 60 cases of dysfunction of the
temporomandibular joint by puncturing zusanli acupoint, Journal of Traditional
Chinese
Medicine, 1993; 13(3): 191.
31. Dang Wen and Yang Jiebin, Clinical study on acupuncture treatment
of stomach carcinoma pain, Journal of Traditional Chinese Medicine 1998;
18(1): 31–38.
32. Kuang Yihuang and Wei Jia, An introduction to the study of
acupuncture and moxibustion in China, part III: Review of clinical studies
on acupuncture
and moxibustion, Journal of Traditional Chinese Medicine,
1984; 4(4): 249–254.
33. Cai Wuying, Acupuncture and the nervous system, American
Journal of Chinese Medicine, 1992; 20(3–4): 331–337.
34. Lin JH, et al. Treatment of iatrogenic Cushing’s Syndrome
in dogs with electroacupuncture stimulation of Stomach 36, American Journal
of Chinese
Medicine, 1991; 19(1): 9–15.
35. Cui Yunmeng and Qi Lijie, Application of zusanli in surgery,
International Journal of Clinical Acupuncture, 1998; 9(3): 317–321.
December 1998
Figure 1.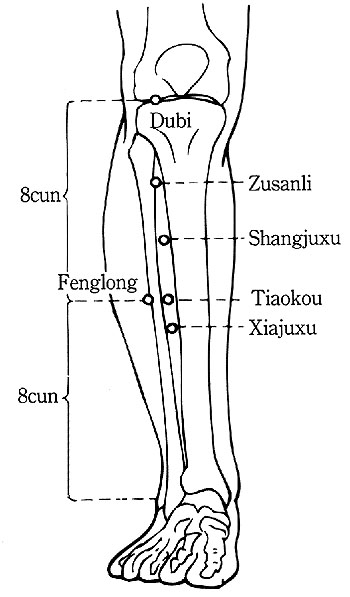
| MX101 | Chinese
Traditional Packed Moxa Rolls - used for indirect moxa heat treatment.
Paper covered rolls are approximately 8.3" x 0.75" in diameter.
|
(+shipping) |

The Dynamics of Disease
How the Ayurveds and Homeopaths
perceive disease.

Sleep and the Inner Landscape,
An Interview about
Dreams and Tibetan Medicine with
the Tibetan Physician, Dr. Yeshe
Dhonden

Medicine Buddha holding myrobalan
|
|
|
|

"Tibetan incense, medicinal powder, and
Tibetan 'precious pills' are in
great demand here," said one police officer who asked not to be
named.
"People believe that it can prevent the virus. And SARS hasn't spread
to Tibet."
Radio Free Asia-May 7, 2003
|
|
|
|



Handbook of Traditional Tibetan Drugs:
Their
Nomenclature,Composition, Use and Dosage
Order
now from our
Secure
Online Order Form
J.Crow Company
PO Box 172
Emerson Hill
New Ipswich, New Hampshire 03071
USA
Fax or Phone
1-800-878-1965 (US & Canada)
603 878 1965 (All Others)
|
|
 Dr.
Jarvis' Unpublished Notebook Dr.
Jarvis' Unpublished Notebook
-147 hand written pages of advice to correspondents- CD-PDF Format $49.95 ea. Includes Shipping |
" I believe the doctor of the future will be a teacher as well as
a physician.
His real job will be to teach people how to be healthy."
Dr.
D.C. Jarvis
|
|
MORE ON MOXIBUSTION
Practical Considerations for Modern Use of an Ancient Technique
After the Chinese revolution in 1949, a great reorganization of traditional Chinese medicine was undertaken. One of the first steps was to investigate and evaluate the traditional methods of acupuncture and moxibustion therapy. The results of such studies were published in a series of reports in the English language Journal of Traditional Chinese Medicine in 1984. In the first article of the series (4), devoted to history of the practices, only the following was noted specifically about moxibustion:
Some fifty kinds of moxibustion methods have been summarized through research into ancient literature on moxibustion. In these [documents] are discussed different materials for moxibustion, various shapes of mugwort cone or roll, materials to be placed between the point on the skin and the burning moxa, and different temperatures and manipulation of moxibustion.
The second part of the series on acupuncture and moxibustion (5) is devoted to the variety of techniques employed currently (e.g., scalp acupuncture, wrist/ankle acupuncture, ear acupuncture, etc.). The article offers the following about moxibustion, with emphasis on the clinical efficacy of scarring moxibustion and attempts to introduce greater use of the other non-scarring methods:
Some units have modified their moxibustion apparatus to facilitate the manipulation. Of the various methods of moxibustion, the ones in common use today are those using moxa cone, moxa stick for warm moxibustion, warm cylinder, and in certain cases, burning [the skin] with moxa. It has been pointed out that moxibustion therapy is especially effective for treating deficiency-cold disease, while it is contraindicated in excess disease and in fever due to yin deficiency. However, some workers have presented clinical cases of febrile disease successfully treated by moxibustion therapy. Ancient medical records support this claim. These workers have explored the problem and declare the banning of moxibustion therapy in febrile disease to be groundless. Still, the two opinions coexist and are debated.
Moxibustion therapy is effective in simple and infantile diarrhea, chronic gastroenteritis, peptic ulcer, bronchial asthma, rheumatism of muscles and joints, neurasthenia, hypertension, menstrual disorders, chronic pelvic inflammation, and climacteric syndrome [menopause]. Definite effect was obtained in the treatment of pulmonary tuberculosis, and thromboangitis obliterans. A report of 182 cases of asthma treated with scarring moxibustion at acupoints selected on the basis of differential diagnosis resulted in a shot-term effective rate of 76.9%, with 70% long-term effective rate on follow-up examination for three years. Other reports claim that scarring moxibustion may markedly lower blood pressure, reduce blood viscosity, and dilate various vessels.
These reports indicate that scarring moxibustion decreases the incidence of fulminant apoplexy by lowering blood pressure. Observation over 17 years of 54 cases of high blood pressure revealed that only 5 suffered from fulminant apoplexy after receiving scarring moxibustion, while 4 out of 12 in the control group did. These results of the therapy are obvious. Experimental and clinical studies have pointed to further health benefits of scarring moxibustion. An example is 299 cases of asthma treated by purulent moxibustion in which 70.6% were effective and 29.1% markedly effective. Abnormal WBC count in 20 cases before treatment were corrected in 19 cases….Animal experiments have showed moxibustion to markedly strengthen the immunity of the organism.
Finally, it should be pointed out that although moxibustion has been extensively used clinically, it has received far less attention than acupuncture, a point deserving some thought.
One can take note of the shift in therapeutic indications for moxibustion from accumulation (a type of excess) with cold to deficiency cold, where moxibustion is considered a means to tonify the deficiency. This shift may reflect a change from using moxibustion as a one-time treatment for dispersion to use of it in repeated daily treatments, since tonification of deficiency often requires prolonged therapy. Scarring moxa, also called purulent moxa, is where severe blistering and ulceration of the site occurs (sometimes with unintended infection of the sore), resulting in formation of a scar. This method reflects the dominant form of moxibustion until very recently; for this reason, many writers translate moxibustion as "cauterization." Instructions for moxa application in the Chinese literature would typically involve repeated burning of numerous small moxa cones on the skin directly, causing blistering or further damage. This type of moxa therapy is not discussed in any detail as part of Western acupuncture training because it is not allowable in Western practice.
The production of useful moxa rolls for indirect heating is a modern technological development, compared to the simple practice of forming moxa wool into small cones by hand. Moxa rolls for indirect treatment were introduced at the end of the Ming Dynasty, but did not become common place until after 1950 when factories were established that could turn out thousands of them daily. Still, traditional doctors were used to employing the standard cones for direct moxa and many of them did not easily make the transition to this other method.
In a report on scarring moxibustion presented at a conference in Beijing in 2000, Wang Kenliang (21) points out that:
Moxibustion sore paste must be applied immediately after the moxibustion in order to protect the injured skin and promote non-bacterial suppuration. In one week after the moxibustion treatment, the exudate becomes more and the sore will suppurate gradually…after more than one month, the pus will disappear and the new flesh will grow, the injured skin will get recovered with only slight scar remaining. The patient must take good rest after suppurative moxibustion treatment and avoid heavy labor and abnormal emotions such as sadness and anger; the patient should also take proper food, limit sexual life, and prevent exposure to pathogenic cold or heat. More nutritious food should be taken such as fresh meat, beans, and fresh vegetables; all these foods help the recovery of the moxibustion sore and remove pathogenic factors….This therapy can treat tuberculosis, bronchial asthma, arthritis, hiccup, facial paralysis, and tuberculosis of the neck lymph.
The author of the Journal of Traditional Chinese Medicine review article brings up point that moxa is used extensively in Chinese clinics but receives far less attention than acupuncture. This comment no doubt refers to limited reports of its use as a primary therapy and one can see from Wang's description that moxa treatment can sometimes be a rather serious ordeal, limiting its use in the large hospitals from which most medical reports are generated. One can speculate about other reasons for its infrequent mention in the literature. Most articles on acupuncture therapy report on complex treatment patterns involving numerous acupuncture points. Needles can be inserted one by one and then the practitioner can perform manipulations on each, leaving them in place for 20-30 minutes. Moxibustion is usually done on only one or two of the points in a complex treatment pattern including acupuncture. As a result, the main part of therapy is the needling, with moxa as a small portion of the treatment. It is difficult for the authors of reports on these treatments to make the proclamation that the therapy is based on moxibustion or that the outcome was reliant on the moxibustion portion of treatment.
Relatively few diseases are treated by moxa alone or with it as the primary therapy. Thus, little attention is given to this technique, in part, because it accompanies acupuncture where the latter is used with more points and with more specific manipulation. Articles on moxibustion as the primary technique tend to be short, and little is said about the point selection or method of applying the moxa. In an article purporting to describe diseases effectively treated by moxibustion (44), three cases are singled out and only one of them (treatment of pterygium) involved moxa alone, the others (carpal tunnel syndrome and throat neuralgia) involved moxa plus acupuncture.
In fact, a search for clinical research on moxibustion in the Journal of Traditional Chinese Medicine (in publication for more than 20 years) revealed few articles on moxibustion, and the majority of the articles that mention this technique made use of it as a seemingly minor adjunct to acupuncture therapy. Articles that mention acupuncture and moxibustion in the title often are merely giving the translation of zhenjiu, while the treatments described involve needling only.
In part 3 of the series reviewing acupuncture and moxibustion (6), with focus on the disorders the various techniques are considered useful in treating, moxibustion is specifically mentioned as successful for one application-correcting abnormal fetal position:
The success rate of moxibustion on zhiyin (BL-67) in checking abnormal fetal position markedly exceeds the figure for manual restoration reported abroad. Two to 4 sessions sufficed, though cases with very loose or very tense abdominal wall, with fixing of the fetal head below the subcostal region, and with partial descent of the fetus into the pelvic cavity were less successful or even ineffective.
The other reports summarized in that review involve either acupuncture alone or "acu-moxibustion," referring to use of acupuncture and possible inclusion of moxibustion in at least some of the treatments (with no mention of specific moxibustion techniques). A rare example of a report in which non-scarring moxibustion was used as a primary therapy for a chronic disease was published in 1992. It involved 183 patients with coronary heart disease. Here is the description of the technique, using moxa rolls:
The acupoints selected included neiguan (PC-6, bilaterally), shenzhong (CV-17), and xinshu (BL-15 bilaterally). During treatment, the patient was in a lying position with full exposure of the acupoints. The ignited end of the moxa roll pointed directed toward neiguan (one side), with the burning end 0.5-1.0 cun away from the skin, for 5 minutes until the patient had a warm but not burning feeling and the skin color turned slightly red. Then, the same method was applied to neiguan of the other hand, shanzhong, and xinshu (both sides), each for 5 minutes. The treatment was given once a day, 6 times constituting one treatment course. There was one day of a rest before the second course of treatment started. The acupoints used for the control group were the same as for the moxibustion group, only acupuncture was used instead of moxibustion….Usually, the patients in both the moxibustion and control groups were given 5-10 courses of treatment, covering a period of 1-2 months.
In their summary, the authors, echoing the comment that moxibustion does not receive much attention, noted that: "In recent years most clinical and experimental studies have proved that acupuncture with neiguan as the main point has good therapeutic effect in the treatment of coronary heart disease; however, few reports on moxibustion in the treatment of this disease have been seen." They also noted that: "There is no significant difference between the moxibustion and acupuncture groups in their effects." Unfortunately, in the absence of a placebo control, it is difficult to know how much of the effects were due to stimulation of the points and how much were due to other factors not specifically related to the treatment (such as responses usually attributed to "placebo effects"). The claimed benefits included relief of symptoms, improvement of ECG, and lowering of blood pressure and blood lipids. In this case, the authors suggested that the indirect moxibustion was preferred by patients over acupuncture because of lack of pain and discomfort (needling in Chinese clinics is far more vigorous than in Western clinics). This is in contrast to the situation with direct moxibustion, which can be more painful than acupuncture; the painful nature of the usual direct moxibustion being mentioned in several texts.
The intensive moxibustion described in this clinical report where moxa rolls were used contrasts with common practice in Western clinics. Moxibustion was given for 5 minutes at each point, with five points treated, for a total of 25 minutes of moxibustion and the treatment was given daily for 30-60 days consecutively. Heating was done until there was an obvious reddening of the skin. In Acupuncture: A Comprehensive Text (27), the importance of adequate heating is mentioned: "A text of the Qing Dynasty, The Golden Mirror of Medicine, explains: 'When treating diseases with moxibustion, for there to be any effect, the heat must be sufficient to obtain the Qi.'"
In another case of treating a chronic disease, herb-interposed moxibustion was administered in the treatment of Hashimoto's thyroiditis (28). Two groups of points were selected for treatment on alternate days: dazhui (GV-14), shenshu (BL-23), and mingmen (GV-4) made up one set; shanzhong (CV-17), zhongwan (CV-12), and guanyuan (CV-4) were in the second set. Each time, five cones of moxa, 2 grams each, were burned continuously on each point of the set. In patients were treated daily, out patients were treated every other day, with a total of 50 treatments for a course of therapy. Many of the patients were said to have benefited in terms of symptoms and findings in blood tests with regard to thyroid hormones and antithyroid antibodies.
References to the use of moxibustion have declined in recent issues of the Journal. Two very brief articles in recent issues described use of moxibustion, both by the herb interposed method, one with ginger, the other with garlic:
Wang Leting, a famous physician in Beijing who practiced from 1929-1979, also commented on using moxa for prolonging life, as described by Dr. Wang's students (22):
The Bian Que Xin Shu (Bian Que's Book of Heart Teachings) says: 'A person without disease should moxa himself for a long time [i.e., regularly]….Although one cannot obtain long life [is not destined to have a long life span], one can achieve longevity of more than 100 years.' Because moxibustion has a warming action and it supports yang, it can be used to course and free the flow of the channels and network vessels, move the qi and quicken the blood, dispel dampness and cold, disperse swelling, and scatter nodulation, secure yang and stem counterflow. For instance, constantly moxaing zusanli (ST-36) is able to regulate and rectify the spleen and stomach function, increase and strengthen the bodily constitution. Constantly moxaing feishu (BL-13), it is not easy to catch an external affliction. Dr. Wang Leting was 88 years old, with the exception of being a little bit hard of hearing, he was still very healthy, his thinking was very keen, and he was still reading and writing books. His secret was mainly doing moxibustion on himself among other methods of protecting his health. He held that after age 40, one's kidney qi declines day by day. Hence, between Summer and Fall every year, when yang qi declines day by day, he began to do moxibustion at qihai (CV-6) and guanyuan (CV-4) with moxa cones. At first, he used 7 moxa cones per day. Then, he gradually used 10 per day and up to a total of 500 for the season. This method greatly strengthened his bodily constitution. He persisted in doing moxibustion for decades and obtained great benefit from it.
The basis for using moxa in the late summer and early fall can be understood by comments in the classics, including the teaching of Li Dongyuan in his Pi Wei Lun (Treatise on Stomach and Spleen). Although Li was an herb specialist and didn't describe use of moxa in this text, he noted that it was traditionally said that diseases of the spleen would heal in the Autumn and that "Blood must be nurtured by all means and the defensive must be warmed by all means. With blood warm and the defensive in harmony, one will live out one's heaven-decreed life span (36)." Moxa provides a warming therapy at this time of year to invigorate the circulation and activity of defensive qi (weiqi) and protect the spleen from the declining yang qi that is occurring as part of the annual cycle, and the blood can be nourished by eating healthy foods, which are digested, and the resulting essence is transported, by the strong spleen function. Failure to take care of this would lead to repeated illness during the cold months, and overall weakening of the body. The important role of the stomach and spleen in generating ying and wei qi helps explain the emphasis on moxibustion at ST-36.
Aside from these uses of moxa for preventive health care, moxa is often applied for alleviating acute symptoms. In an attempt to relieve herpes zoster outbreaks, moxibustion was applied to dazhui (GV-14). According to the report of this application (23), the technique to be used would depend on the patient: for the elderly and weak, warming moxibustion (using a moxa roll) was administered, but for the strong and robust, direct moxa (9 cones, but non-blistering) was done. Treatment was given once per day, with pain alleviation and change of the zoster lesions to scabs occurring in 3-7 days of treatment. A report on moxibustion for gastric spasm by Song and Zhu (12) in the Journal of Traditional Chinese Medicine involved 97 patients with either gastric spasms or intestinal spasms who were treated primarily on the abdomen points CV-8 (along with ST-37 for intestinal spasm) and CV-12 (along with ST-34 for gastric spasm). The authors report that nearly all the patients had their abdominal pain alleviated with one moxa treatment. The technique used was:
The moxa roll was ignited and placed over the selected points to produce a comfortable warm feeling. When the heat became excessive, the moxa roll was moved around the points or a little higher to avoid burns. A piece of gauze could be laid over the point to protect the skin from accidental injury. 30 minutes constituted one session of treatment.
Unlike the concern expressed here to keep the patient comfortable and uninjured, many traditional moxa specialists (such as Wang Kenliang, quoted previously) believed that blistering of the skin was essential to the success of moxibustion when treating serious ailments, much the way that getting the qi reaction and propagated sensation in response to needling was deemed essential to successful acupuncture therapy. This blistering and scarring method is even mentioned in relation to Keeping-fit Moxibustion, which is for preventive health care. Such intensive moxibustion is avoided in the Western practice, which follows more closely the method used for the gastric and intestinal spasm treatments.
|
Smokeless moxa is a rod of charcoal impregnated with
moxa. It burns hot, but slowly, at an average rate of just 2.7 inches per
hour; the rods are about 4.5 inches long, so the total burning time is
about 90 minutes before the rod becomes too short to use. The moxa is not
easily lit, so it is common to use a torch rather than a simple lighter.
Once lit, it burns consistently.
|
|
The smokeless moxa pole produces ash at the burning end
which tends to stick to the rod. When trying to safely remove the ash from
smokeless moxa, the stick should not be tapped against something (e.g.,
against an ashtray). The tapping, aside from making undesired noise, can
crack the charcoal, generating a risk for a piece to fall off and burn
the carpet, treatment table, or patient. Instead, the burning end of the
moxa stick should be gently rubbed against the top edge and inside of a
moxa extinguisher, which will be a quiet operation that dislodges the ash
and does not crack the moxa rod.
|
The moxa extinguisher can be carried in an ashtray, so
that the ash is contained. At the end of the moxa session, the moxa stick
may be carefully retained while still burning for use with another patient
(if it is to be used within minutes) or put out. It is important to check
from time to time that all moxa rods are in their proper place so that
none are left burning where they can cause damage.
|
Moxa can be carried out using a single pole to provide
intense heat to a specific point, or with two poles held side by side to
heat a larger area. Moxa may be applied to acupuncture needles, but take
care not to hold the lit end near the plastic holders, as this can cause
melting or evaporation of the plastic (or rely on metal handle needles).
While a brief moxa treatment can feel good to the patients, all Chinese
texts refer to prolonged heating, usually by repeated application of heat
to the same site over a period of several minutes. Be careful not to lose
most of the potential benefits by applying moxa for a very brief period
or by trying to apply moxa to too many sites, so that each site is only
briefly treated.
|
|
In contrast to the intense direct heating of points
for treating diseases, heat therapy may also be employed to relax tense
muscles and gently relieve aching and mild pain. Self-heating moxa pads
for these purposes have been available from Korea for more than 20 years.
This technology involves having a bag of mugwort and charcoal with an oxygen-sensitive
system (iron that reacts strongly with oxygen), so that when the sealed
package containing the bag is opened and the bag of material is vigorously
shaken for a moment, it heats up. Within five minutes, the pack is heated
and it maintains a temperature of 60-75°C (140-165°F) for hours.
This is the same technology used for the popular new drugstore products,
such as ThermaCare, which are self-heating pads applied to the body (but
without the artemisia).
|
Typical applications of the moxa pads include treatment
of injuries, back pain, knee pain, and menstrual pain. In addition, these
pads are applied for chilliness and discomfort following exposure to excessive
air conditioning, frigid outdoor winter conditions, or damp windy weather.
A belt to hold the pad over the abdomen is also available. The pads can
be used following a treatment with acupuncture and moxibustion to extend
the effects of the initial therapy, or as an alternative to those treatments
when professional help is not convenient. Moxa pads should not be applied
to skin that is broken or to areas that display red inflammation or that
develop greater discomfort with application of heat.
|
Another method of applying heat is the infra-red heat
lamp; a useful variant of this was developed in China, called the "TDP-lamp."
It was invented in 1980 by a group of scientists and physicians headed
by Dr. Gou Wenbin at the Chinese Medicine Institute in Chongqing. Unlike
conventional infrared therapeutic devices, the TDP device features a plate
coated with a mineral formation (a low conductance metal with diverse composition).
When heated by an electric heating element, the mineral plate emits waves
in the infrared range. It produces a uniform heating that makes it more
useful than ordinary glass bulb lamps. To increase the heating of a region
by the lamp, a medicated oil can be rubbed on the skin; the oil helps retain
the heat and its herbal constituents may contribute to the improvement
of local blood circulation. Although the makers of the TDP lamp make claims
about the special value of its frequency of infrared emissions, there is
no evidence that it performs a unique function on this basis.
|
|
|
| MX101 | Chinese
Traditional Packed Moxa Rolls - used for indirect moxa heat treatment.
Paper covered rolls are approximately 8.3" x 0.75" in diameter.
|
(free shipping) |

"You inquired,
as I recall, whether one may permissibly manufacture sweet cider and then,
after natural fermentation has occurred,
sell the finished product,
without complying with the statutory provisions and local regulations governing
the sale of alcoholic beverages."

The way a crow
Shook down on me
The dust of snow
From a hemlock tree
Has given my heart
A change of mood
And saved some part
Of a day I had rued.
Robert Frost

Scene Near Northwood Narrows, NH circa 1918
"Do not believe in anything simply because you have heard it. Do
not believe in anything simply because it is spoken and rumored by many.
Do not believe in anything simply because it is found written in your religious
books. Do not believe in anything merely on the authority of your teachers
and elders. Do not believe in traditions because they have been handed
down for many generations. But after observation and analysis, when you
find that anything agrees with reason and is conducive to the good and
benefit of one and all, then accept it and live up to it.”
Siddhartha Gautama Buddha